Building Effective Care Coordination Software: Key Steps, Features & Best Practices
This guide walks you through everything about care coordination software, from core features and compliance to cost, ROI, and future trends. Learn how the right development partner can help you modernize your healthcare ecosystem.

If you are a health-tech startup, a clinic, or a hospital, chances are you are struggling with one of these:
- Patients are lost in fragmented care journeys.
- Rising readmissions and costs.
- Clinicians are overloaded with manual processes.
- Outdated hospital systems
These are some challenges that healthcare leaders across the world are working on every day.
That’s exactly where care coordination software (CCS) becomes a solution. It breaks down silos, connects every stakeholder, and ensures no patient is left behind.
This blog serves as your roadmap to understanding what CCS can do and how to design it effectively. Implement it effectively with a trusted healthcare software development partner and achieve success.
Table of Contents
What is Care Coordination Software?
Care coordination software is a digital platform that helps doctors, nurses, patients, and caregivers stay connected. Using the platform, they can share the right information at the right time.
The software makes the entire care journey smoother by streamlining information. No chasing records or missing follow-ups. Patients get better outcomes, healthcare professionals save time, and healthcare organizations reduce costs.
What Gaps Does CCS Solve?

- Fragmented data across providers → incomplete patient history.
- Duplication of care (unnecessary tests, overlapping treatments).
- Poor transitions → hospital discharge to home care often fails.
- High readmissions → preventable with proper follow-up and monitoring.
- Administrative overload → clinicians spend hours chasing information instead of patients.
Key Features of Care Coordination Software
A well-designed Care Coordination Software (CCS) should have clinical functions, operational efficiency, and be effective for patients.
Here is a table of the core vs. advanced features you should consider when developing or implementing CCS.
| Category | Core Features (Must-Have) | Advanced Features (Future-Ready) |
| Patient Management | Centralized patient record (demographics, history, SDoH) | Remote Patient Monitoring (IoT devices, wearables) |
| Care Planning | Care plan creation, goal setting, progress tracking | AI-driven personalized care recommendations |
| Workflow & Tasks | Task assignments, referral tracking, alerts | Multi-institution collaboration tools |
| Scheduling | Appointment scheduling, calendar sync, reminders | Smart scheduling with AI optimization |
| Communication | Secure messaging, video/telehealth, provider-patient chat | Multilingual, WCAG-compliant, accessibility-first interfaces |
| Integrations | EHR/EMR (HL7, FHIR, telehealth, lab systems) | Blockchain-enabled data integrity & cross-border data flows |
| Analytics | Dashboards for outcomes, compliance, and cost metrics | Predictive analytics & risk stratification with AI/ML |
| Patient Engagement | Patient portal, mobile apps, reminders, education resources | Gamification & AI-based nudges for adherence |
| Security & Compliance | HIPAA/GDPR compliance, role-based access, MFA, encryption | Advanced certifications (ISO 27001, SOC 2), audit trails |
| System Flexibility | Web + mobile provider/patient views | Offline mode for rural/low-bandwidth regions |
1) Core Features (Essential for Every CCS)
These are the must-have modules that form the foundation of a care coordination platform.
-
Patient / Client Data Management
Centralized record of demographics and medical history. It has details of the patient’s medications, allergies, and social determinants of health (SDoH).
-
Care Plan Creation & Management
You can set care goals using this feature. And assign responsibilities to the relevant task manager or employees. It becomes easier to track progress and update plans dynamically.
-
Workflow, Task & Referral Management
With this feature, you can automate task assignments. It helps with referral tracking. Timely alerts ensure that no patient falls through the cracks. Facilitates on-time care for patients with the application.
-
Scheduling & Calendar Management
A great option for scheduling appointments across various providers. There is an option for reminders and resource availability tracking. Through which you can easily manage the resources at hand.
-
Communication & Collaboration Tools
When using care coordination software, communication becomes of utmost importance. Secure messaging, chats between provider and patient, and team alerts.
-
EHR/EMR & Third-Party System Integrations
HL7/FHIR supports interoperability with hospital systems. It also supports labs, imaging, and telehealth platforms.
-
Analytics & Reporting Dashboards
Getting detailed information in the form of analytics makes it easier for the healthcare professional/provider to understand the issue. Performance insights and referral tracking are some great options. You can get outcome monitoring and compliance reports that help with better care provision.
-
Patient Engagement Interfaces
Patient portals, mobile apps, and reminders are some great ways to keep the patient informed and allow them to enter their details. It helps in maintaining basic information in one place. Education resources to keep patients actively involved and give information about the situation.
-
Security, Privacy & Compliance Modules
To secure your app and data, you can choose from role-based access and multi-factor authentication for security. When you need encryption, you can choose from various algorithms like SHA and AES-256. Healthcare regulations like HIPAA/GDPR compliance are mandatory.
2) Advanced Features (For Enterprise & Future-Ready CCS)
These features differentiate an advanced CCS from an enterprise-level platform.
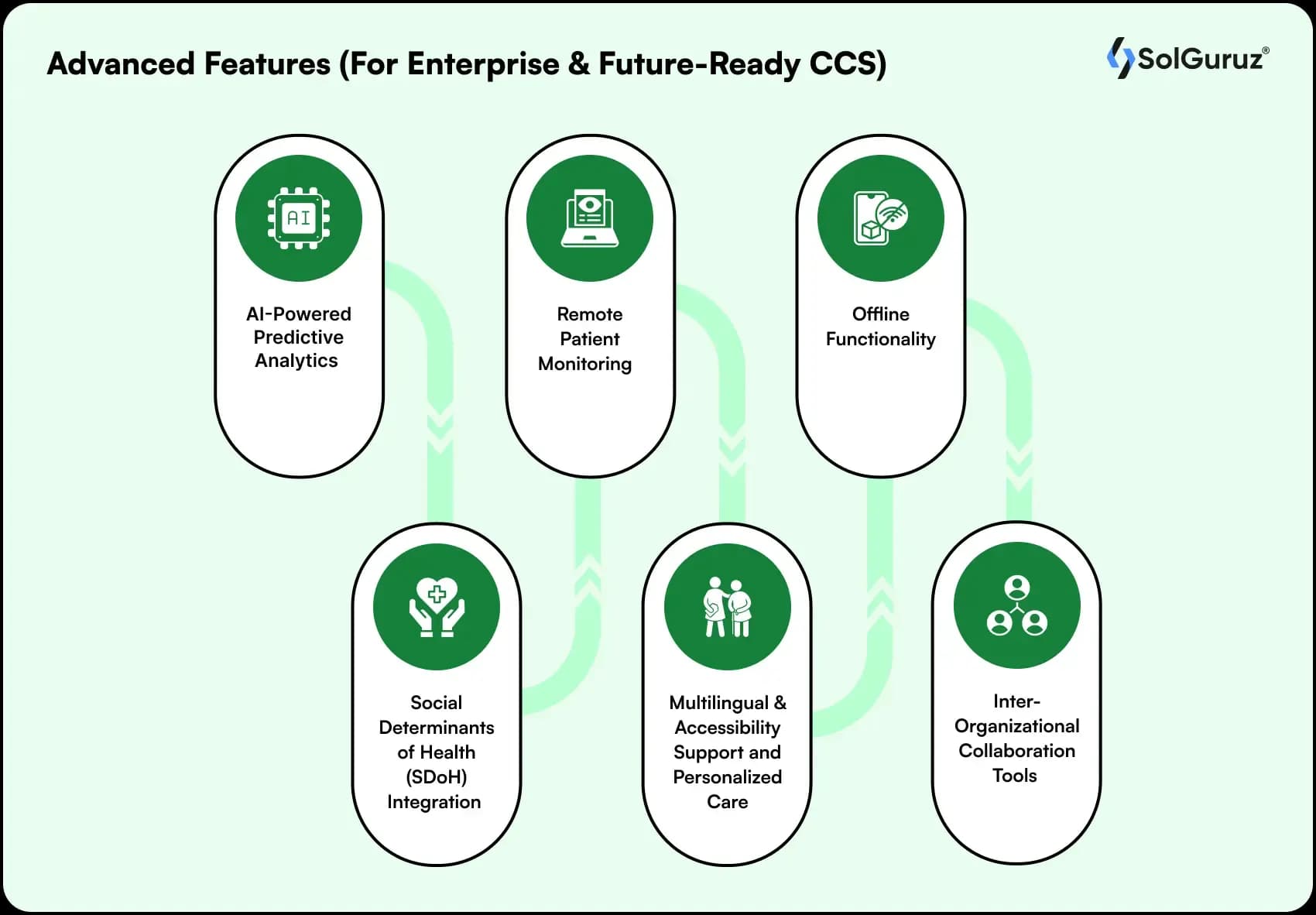
-
AI-Powered Predictive Analytics
You can use machine learning models for identifying high-risk patients. Also, AI can be used to predict readmissions and recommend interventions. AI/ML in the healthcare industry can help improve the systemic flaws.
-
Social Determinants of Health (SDoH) Integration
Adding social, economic, and environmental data to improve the overall care. It helps with giving healthcare a holistic approach.
-
Remote Patient Monitoring
Using IoT devices and wearable integration like BP cuffs, glucometers, and heart monitors. These devices provide real-time data flow into CCS.
-
Multilingual & Accessibility Support and Personalized Care
Accessibility-first interfaces and multi-language support make your software more accessible and acceptable. Personalized care, like personal notifications or reminders ,will be the next thing in the future.
-
Offline Functionality
Offers care coordination in rural or low-bandwidth environments. With sync-on-connect capabilities, the software can be used in lower-bandwidth areas.
-
Inter-Organizational Collaboration Tools
With this feature, you can share records and workflows for multi-institutional care. It helps institutes like hospitals, community clinics, and insurers.
How to Use This in Your Project:
Core features = the foundation of every Care Coordination Software MVP.
Start with core features in your MVP (patient data, care plans, workflows, communication, EHR integration).
Advanced features = the differentiators for enterprise adoption & future scalability.
Add advanced features gradually as you scale or target specialized use cases (AI, IoT, multilingual, predictive care).
Once you have finalized the features, move on to choosing the architecture of the software.
Technology & Architecture Considerations for Care Coordination Software
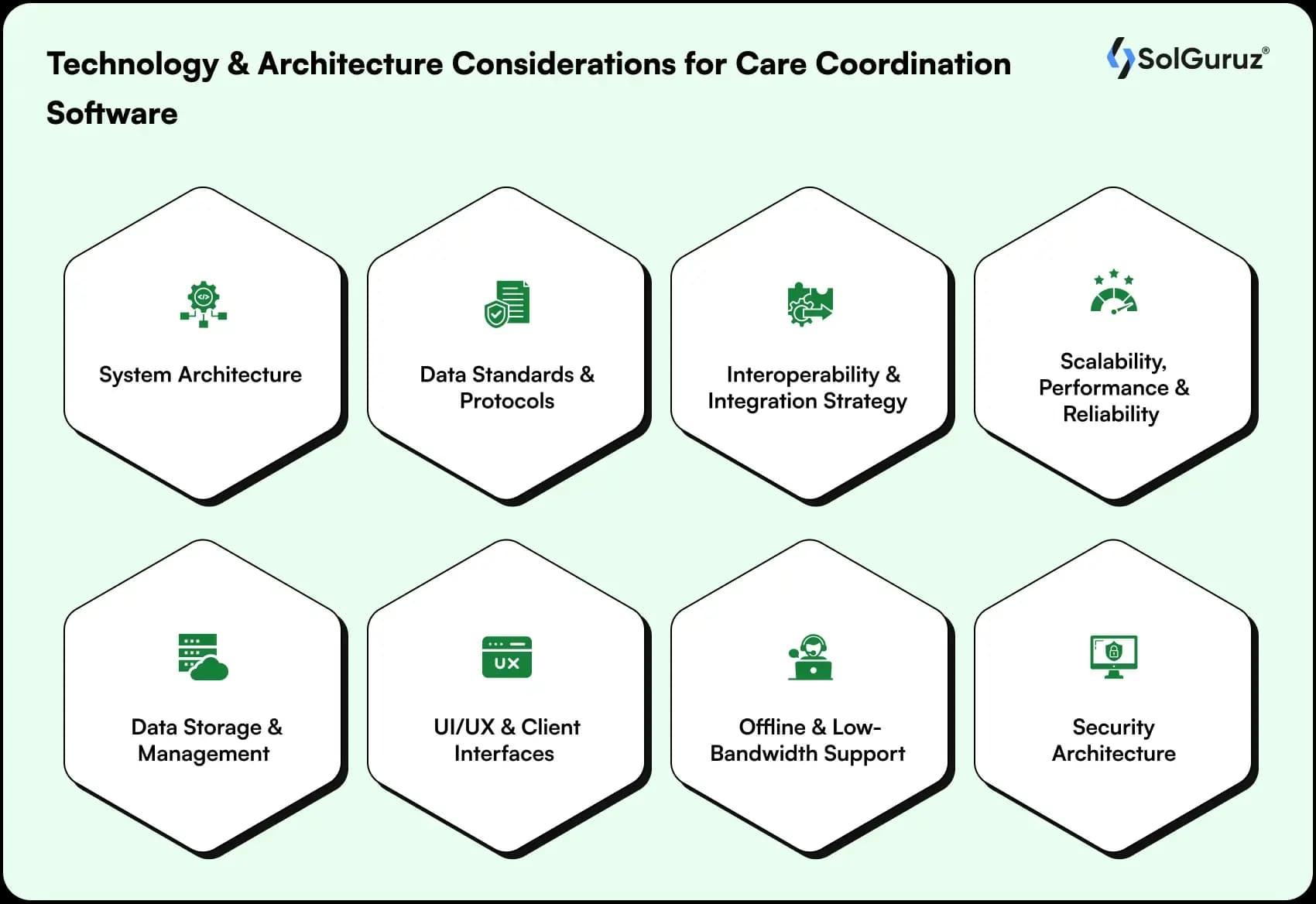
Designing and implementing Care Coordination Software (CCS) is not just about features. It is about building a scalable and secure healthcare ecosystem. Below are the critical considerations:
1. System Architecture
Monolithic:
- All components (UI, backend, data, and integrations) are bundled in one system.
- Simpler to build initially.
- Harder to scale, maintain, and integrate with new modules.
Microservices:
- Independent services for scheduling, care plans, communication, etc.
- Scalability, faster updates, better fault isolation.
- Requires stronger DevOps and orchestration, like Kubernetes.
Modular / API-First:
- Each module, like EHR integration or patient engagement, can be treated as an API.
- Works great for third-party integrations, SaaS deployment, and making future-ready software.
- More upfront design effort.
2. Data Standards & Protocols
A few widely accepted standards that CCS must comply with are:
- FHIR (Fast Healthcare Interoperability Resources) → for structured healthcare data exchange with modern tech like RESTful APIs or JSON formats.
- DICOM (Digital Imaging and Communication in Medicine) → Used for medical image retrieval, transmission, and storage. Mostly used for imaging workflows in radiology
- X12 / EDI (Electronic Data Interchange) → A standard for business transactions for financial and administrative purposes. Used for insurance claims and billing.
3. Interoperability & Integration Strategy
For better integration, you can integrate these platforms or APIs into your software for a smoother UX.
- EHR/EMR Integration → While integrating EHR, the software must connect with major hospital systems like Epic, Cerner, and Meditech.
- Telehealth Platforms → Zoom, Doxy.me APIs for smooth video calls or telecalls.
- Labs & Diagnostics → LIMS integration for test results. This helps patients to see their test results with a tap.
- Pharmacy Systems → For e-prescriptions and medication tracking.
External APIs → Wearables like Fitbit or Apple Watch, or IoT devices for chronic care monitoring.
4. Scalability, Performance & Reliability
Healthcare data and coordination involve large-scale concurrent users (clinicians, patients, administrators).
- Load Balancing & Auto-Scaling → for peak demand (e.g., pandemic surges).
- Caching & Queue Systems → to handle referral requests, notifications, and task queues.
- Real-Time Updates → WebSockets/SignalR for instant alerts and task changes.
5. Data Storage & Management
For data storage, you have two options – structured data and unstructured data:
- Structured Data → Clinical information like lab results, vitals, and medications is stored in relational DBs. Mostly used databases are PostgreSQL, MySQL, and MS SQL.
- Unstructured Data → Notes, images, and discharge summaries are counted as unstructured data. These are generally stored in document DBs like MongoDB and CouchDB.
- Data Lakes → They are used for analytics and population health management.
- Cloud Options → AWS HealthLake, Azure for Healthcare, Google Cloud Healthcare API. These cloud options are built for HIPAA/GDPR compliance.
6. UI/UX & Client Interfaces
Different stakeholders (clinicians, patients, and admin staff) require tailored interfaces. We have shown which interface is most useful for whom.
(This will be helpful when you are designing and wireframing your care coordination software.)
- Clinicians → Dashboard for tasks, patient charts, care plans, referrals.
- Patients → Simple, mobile-first portal with reminders, education resources, and telehealth access.
- Admin Staff → Scheduling, reporting, compliance tools.
- Accessibility → WCAG-compliance, multi-language support, voice commands for aging populations.
7. Offline & Low-Bandwidth Support
This important architectural feature is critical for rural, underserved, or low-resource environments. Places where there is no internet availability or very little internet connection. What will work is:
- Local caching with sync-on-connect strategies.
- Lightweight, mobile-first design that works even with poor network coverage.
- Offline facilities like downloads, which once downloaded, can be opened without an internet connection.
8. Security Architecture
Healthcare is a high-risk target for cyberattacks. Your care coordination software must include:
- Data Encryption: You can use data encryption algorithms for End-to-end encryption (AES-256). Also, you can use TLS 1.3 for in-transit data.
- Access Control: It is a good measure to control security. Role-based (RBAC) and attribute-based (ABAC) permissions control information leakage to a greater extent.
- Authentication: Multi-Factor Authentication, Single Sign-On SSO, or OAuth2 are some of the authentication methods. These methods are used for identity authentication and to avoid identity theft.
- Audit Trails: Regular audits help in avoiding any threats. You can track the actions of users to keep things in check.
- Threat Protection: Regular vulnerability scans and penetration testing work like magic for healthcare apps. The scans show you threats that you can easily resolve to protect your software.
Compliance, Privacy & Regulations
Building care coordination software (CCS) means handling highly sensitive patient data. To ensure trust, safety, and adoption, you can not compromise on security or compliance.
A quick glance through a table of various compliances, the region, what they require, and their impact on the CCS.
| Regulation / Certification | Region | What It Requires | Impact on Care Coordination Software (CCS) |
| HIPAA (Health Insurance Portability and Accountability Act) | United States | Protection of PHI, data encryption, secure transmission, and strict access control | CCS must implement encryption, audit logs, role-based access, and secure communication channels. |
| GDPR (General Data Protection Regulation) | European Union | Consent management, right to be forgotten, data portability | CCS must provide clear opt-ins, patient data export, and deletion features to comply with EU privacy laws. |
| 21st Century Cures Act | United States | Mandates patient access to electronic health data, encourages interoperability | CCS must support APIs and standards like FHIR to allow patients and providers to access and share records. |
| DISHA (Digital Information Security in Healthcare Act) | India | Regulates the collection, storage, and exchange of digital health data | CCS deployed in India must include consent management, secure storage, and auditability for patient records. |
| PIPEDA (Personal Information Protection and Electronic Documents Act) | Canada | Governs how personal health data is collected, used, and disclosed | CCS must ensure explicit consent and data storage compliance when operating in Canada. |
| ISO 27001 | Global | International standard for Information Security Management Systems (ISMS) | Certification shows CCS follows best practices for securing healthcare data, boosting trust. |
| SOC 2 | Global (popular in US/EU enterprises) | Framework for data security, confidentiality, and privacy | Certification assures clients that CCS handles sensitive data responsibly, supporting enterprise adoption. |
Here’s a quick breakdown of the major frameworks and certifications:
-
HIPAA (US)
The HIPAA safeguards Protected Health Information (PHI). The software must have data encryption, access control, and secure data exchange to stay HIPAA compliant.
-
GDPR (EU)
The General Data Protection Regulation focuses on user consent, data portability, and the “right to be forgotten.” For EU patients, CCS must allow clear opt-ins and data transparency. It should allow patients to request the deletion of their personal records.
-
21st Century Cures Act (US)
This regulation mandates open patient access to their health records via APIs and electronic systems. Care coordination software should support interoperability standards like FHIR to give patients more control over their data.
-
Local Regulations
Each region has its own healthcare data laws – for example,
-DISHA in India governs digital health data privacy and health records.
-PIPEDA in Canada sets guidelines on collecting, using, and disclosing personal health information.
When working in different geographies, following local rules becomes essential for deployment.
-
Certifications
These are global standards for practicing strong data security practices. Given to organizations following the data security rules. Certifications reassure patients and other businesses about the standards being followed.
-ISO 27001 ensures robust information security management. SolGuruz is ISO certified and follows robust data security practices.
-SOC 2 confirms that your software follows strict controls for privacy, availability, and confidentiality-boosting enterprise trust.
UI/UX Design & Usability for Different Stakeholders
Design and usability are important in care coordination software, since different stakeholders have different needs. What different stakeholders can expect:
1) Clinicians: Doctors and nurses need to focus on patient care, not on navigating complex menus. Smart shortcuts, intuitive workflows, and role-based dashboards make adoption easier for them.
What will help – Easy navigation.
2) Patients: Simplicity is key. Patients love mobile-friendly interfaces, with multi-language support. The software should meet WCAG accessibility standards to support users with disabilities.
What will help – Clear icons, reminders, and self-service tools to improve patient engagement.
3) Administrators: They need powerful yet intuitive dashboards to track workflows. Data visualization and drill-down reports help in quick decision-making. They also need to track resource allocation and compliance.
What will help – Data visualization reports
4) Adoption: Smooth onboarding and structured training help in greater adoption. A phased rollout of the software helps reduce resistance.
What will help – Feedback loops improve usability over time.
Worth reading – Steps to develop a healthcare staffing app, if you want to build a staffing app for healthcare professionals.
How to Develop a Care Coordination Software?
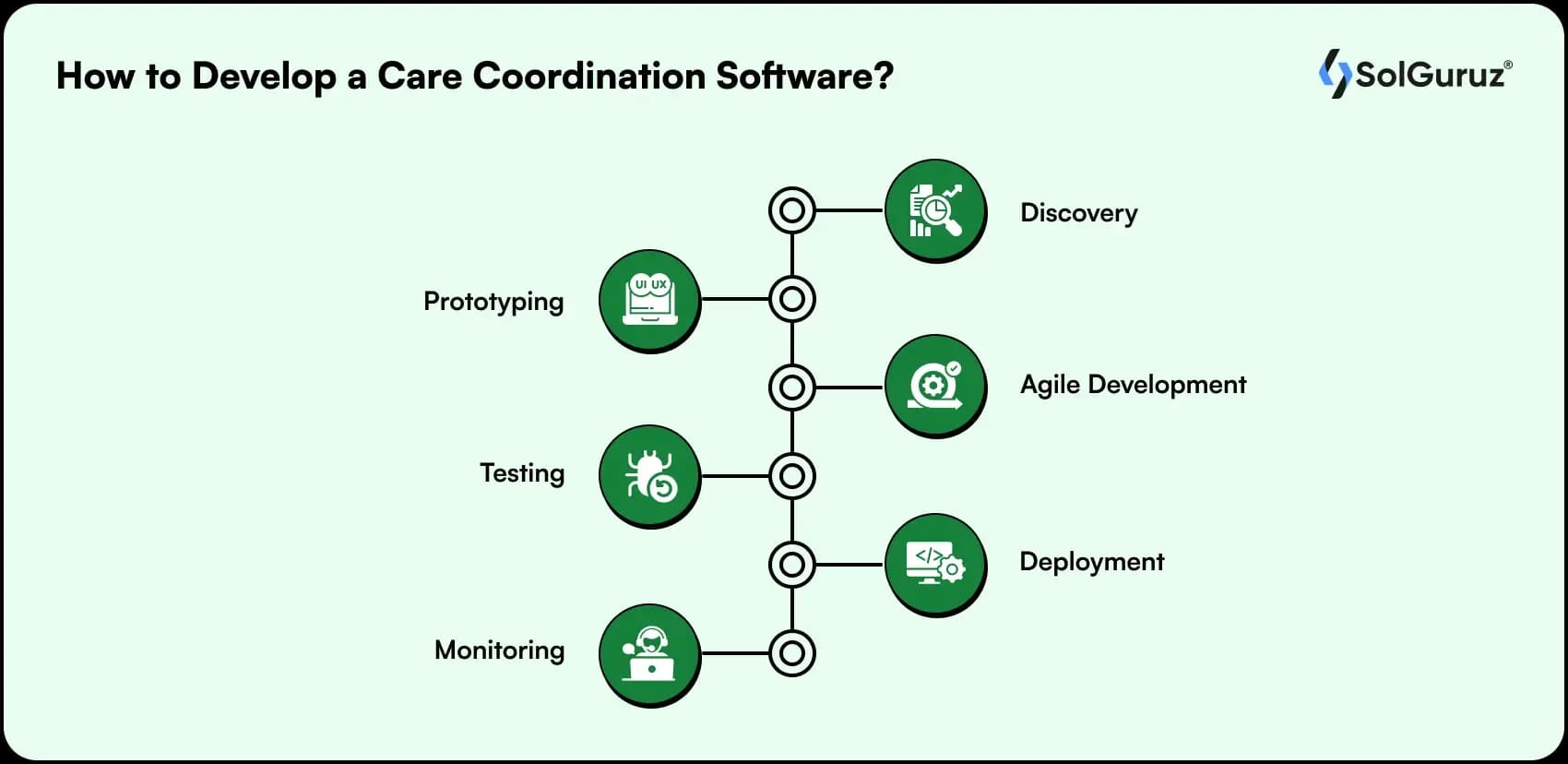
Building successful care coordination software CCS requires a structured approach. Partnering with the right healthcare software development company becomes a necessity.
1. Discovery – This phase includes interviews and pain point mapping. It helps us identify gaps in current systems and client requirements. This step defines the requirements for clinicians, patients, and administrators.
2. Prototyping – Depending on the scope, teams can start with an MVP (Minimum Viable Product)development. MVP development validates the key features and gives you an idea of whether to go for a full build. Also, prototyping reduces risks by making sure that the user feedback is incorporated early. We advise clients to go for an MVP build first, which reduces the risk involved.
Also read: How to develop an AI MVP to launch within a week.
3. Agile Development – Using Agile and DevOps practices, developers implement CI/CD pipelines for faster, more reliable delivery. Using this approach ensures modular builds and quick iterations. Also, making sure that there is continuous improvement throughout the healthcare software development process.
4. Testing – Rigorous testing covers usability, integration with EHR, performance under load, and security compliance, such as HIPAA and GDPR. Functional and non-functional testing make it easier to find and fix bugs. It ensures the software is both safe and reliable for healthcare environments.
5. Deployment – The software can be deployed on cloud, on-premises, or hybrid models. It all depends on the healthcare organization’s needs for scalability, data residency, and compliance. Though deploying on the cloud reduces the infrastructure costs.
6. Monitoring – Continuous monitoring allows for bug fixes, system updates, and security patches. Feedback-driven improvements ensure long-term reliability and adaptability of the care coordination system.
Cost & Timeline Estimates for Care Coordination Software
The cost and development timeline of a care coordination solution depend on the complexity, integrations, compliance, and scalability needs. Below is a benchmark table for quick reference:
| Project Size | Estimated Cost (USD) | Timeline | Best Fit |
| Small / Basic CCS | $25,000 – $40,000 | 3–4 months | Small clinics, startups with limited workflows |
| Mid-Sized CCS | $40,000 – $80,000 | 6–9 months | Regional hospitals & specialty providers |
| Enterprise CCS | $150,000+ | 12–18 months | Large health networks & insurers needing advanced features |
Key Cost Drivers
- Integrations: EHR/EMR, telehealth, IoT devices, lab systems.
- Compliance Needs: HIPAA, GDPR, or multi-region regulations increase testing or security costs.
- Scalability & Performance: Building for thousands of concurrent users requires robust cloud infra like AWS, Azure, GCP.
- Features & Customization: AI-driven insights, multilingual support, and advanced analytics add to the budget.
Measuring Success: KPIs & ROI
The effectiveness of care coordination software (CCS) should be proven with measurable results. Tracking the right KPIs allows healthcare providers, payers, and administrators to quantify improvements in both patient care and financial performance.
Key KPIs to Track
- Reduced Readmissions
Smoother care transitions and proactive follow-ups lower avoidable readmissions. This results in saving hospitals from penalties and hence saving some costs.
- Faster Referrals
Automated referral management makes sure patients receive timely specialist appointments. Resulting in reduced care delays, improving patient care.
- Higher Patient Satisfaction
Multilingual portals, real-time communication, and reminders empower patients. And hence improving compliance and overall care experience.
- Better Clinician Productivity
CCS eliminates repetitive documentation and streamlines workflows. This, in turn, allows clinicians to focus on direct patient care.
- Lower Duplicate Tests & Costs
Interoperability with EHR/EMR allows visibility into patient history, preventing redundant imaging or lab tests.
ROI Framework for CCS

Organizations can measure ROI (Return on Investment) by comparing savings and improvements against the cost of implementation and operations.
| Scenario | Benefit | Cost Impact | ROI Example |
| Readmission Reduction | Avoiding 100 readmissions per year at $15,000 each | $1.5M saved | If CCS costs $250K/year → ROI = 500% |
| Duplicate Test Reduction | Preventing 500 duplicate tests at $200 each | $100K saved | If CCS costs $250K/year → ROI = 40% |
| Productivity Gains | Clinicians save 2 hours/day → worth $80K annually | Reduced overtime/staffing | Direct operational savings |
| Patient Retention | Higher satisfaction = 10% retention boost | Long-term revenue growth | Hard ROI + brand credibility |
By aligning CCS investment with measurable financial, operational, and clinical KPIs, healthcare providers can demonstrate not just compliance but clear value.
Now, it is necessary to know the “Do’s and Don’t’s” before starting your care coordination software development.
Challenges and Best Practices

A good partner will not only guide you where to go but also what not to do. Here we have compiled a list of challenges that you might face during your CCS process. So, prepare them beforehand.
Key Challenges
- Stakeholder Misalignment
Clinicians, administrators, and payers may have different expectations from care coordination software. Without a shared vision, projects can stall or face resistance.
- Data Silos
Healthcare data is often locked in separate systems (EHRs, labs, imaging platforms). Lack of interoperability makes it hard to create a unified patient view.
- UX Adoption Issues
If the software is too complex, clinicians and patients won’t use it effectively. High cognitive load and poor onboarding often lead to low adoption.
- Complex Integrations
Integrating CCS with EHRs, telehealth platforms, and IoT devices is technically demanding and can increase project timelines if not planned early.
Best Practices
Best Practices for CCS Development
- Start with an MVP
- Prioritize UX for easy workflows.
- Ensure compliance early, like HIPAA or GDPR.
- Use modular design for scalability & integrations.
Case Studies & Success Stories
Here are the real-world scenarios where our custom healthcare software development solved some of the challenges.
Shift Squad is a powerful AI-powered Healthcare Staffing App. The staffing app helps the healthcare industry in nurse staffing and recruiting other healthcare professionals.
Generally, healthcare agency apps should adhere to regional compliance requirements. Our goal was to create a secure and compliant app. We developed Shift Squad as a HIPAA-compliant app with robust data security measures.
The result was a quick and intuitive nurse staffing app, featuring the latest technology, including AI and healthcare staffing solutions. The application can assist you with both temporary and permanent staffing solutions through smart recruiting options. An intuitive staffing module with a user-friendly healthcare staffing web design.
Future Trends in Care Coordination Software in 2025 & Beyond
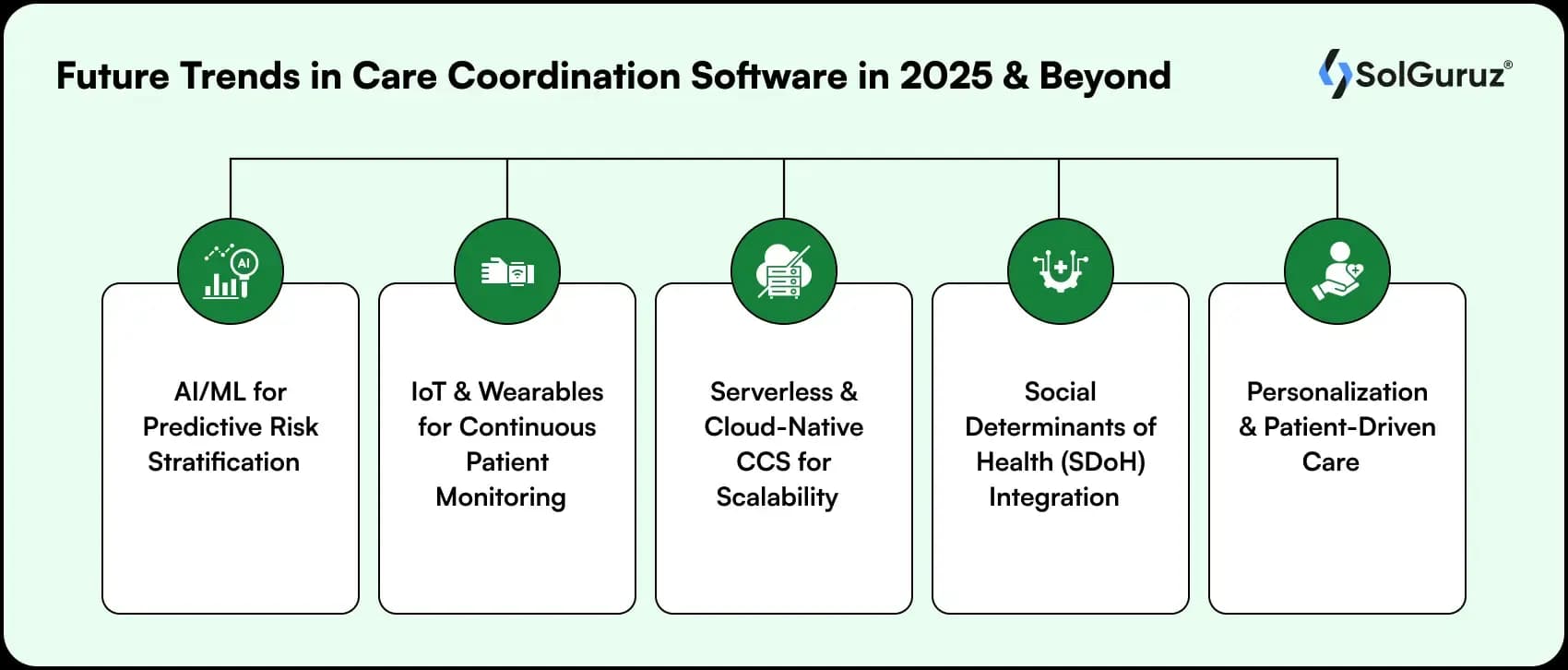
With the latest tech changing the healthcare industry, the future holds some intuitive patient care measures. Here are some trends that are creating waves in the healthcare industry in 2025 and will continue in the future.
AI/ML for Predictive Risk Stratification
AI-driven analytics will help identify high-risk patients earlier. Data-backed predictions reduce readmissions and personalize care plans.
1. IoT & Wearables for Continuous Patient Monitoring
Smart devices like wearables and remote monitors help with real-time health tracking. This improves chronic disease management and proactive interventions.
2. Serverless & Cloud-Native CCS for Scalability
Healthcare organizations will increasingly adopt serverless and cloud-native architectures. It handles large volumes of data securely while reducing infrastructure costs.
3. Social Determinants of Health (SDoH) Integration
Integration of SDoH factors like housing, environment, and income helps in giving better results. It helps clinicians to understand and work on the root cause of the problem. This offers a more holistic, whole-person care approach.
4. Personalization & Patient-Driven Care
More personalized care will be available in the future. Patients will expect a tailored care experience with the latest tech involved. Multi-language apps, custom care plans, and greater control over their health data.
Need an Expert Care Coordination Software Development Partner?
When building a care coordination software solution, it is not just about coding – it demands deep expertise in healthcare workflows, compliance, and scalable technology.
At SolGuruz, we specialize in crafting tailored healthcare software that bridges gaps between providers, patients, and payers.
Our team helps you:
- Translate complex clinical workflows into intuitive digital solutions.
- Build HIPAA- and GDPR-compliant systems from day one.
- Design scalable, API-first architectures ready for integrations with EHRs, IoT, and telehealth platforms.
- Deliver user-friendly experiences for clinicians, patients, and administrators.
Whether you’re a small clinic, a regional hospital, or a global healthcare network, we bring the right mix of technical depth, healthcare expertise, and agile delivery to your project.
Looking to build or modernize your care coordination software?
Let’s discuss how SolGuruz can help turn your vision into a secure, scalable, and patient-centered reality.
FAQs
1. Who uses Care Coordination Software?
Doctors, patients, caregivers, hospital administrators, and payers use care coordination software. It helps in smooth care transitions, avoiding the duplication of tests, and managing chronic conditions effectively.
2. What are the Key Features of Care Coordination Software?
Some of the core features include patient data management, EHR integration, and referral tickets. Advanced features may include AI-driven features or IoT wearables.
3. How Much Does it Cost to Develop a Care Coordination Software?
Basic software with basic features will cost approximately $25000. For details, you can refer to the cost section of the blog.
4. Do You Need HIPAA or GDPR Compliance for Care Coordination Software?
Yes, any healthcare software must be compliant with regulations. HIPAA for the US, GDPR for the European Union, and DISHA for India. You should ask the healthcare software development company for the details of their compliance.
5. What are the Benefits of Care Coordination Software?
The major benefit is patient satisfaction. Other benefits include reduced hospital readmissions and faster referrals, which improve patient care.
Build a Patient-Centred Care Software
Struggling with siloed healthcare systems? Partner with SolGuruz to design scalable, compliant, and patient-focused care coordination software.

Strict NDA

Trusted by Startups & Enterprises Worldwide

Flexible Engagement Models

1 Week Risk-Free Trial
Give us a call now!

+1 (724) 577-7737



